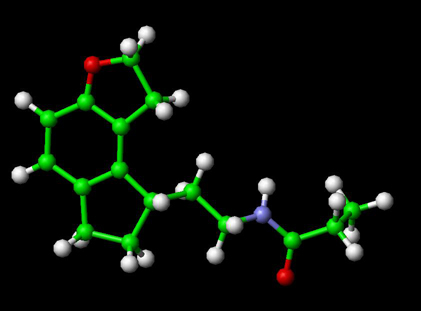
Ramelteon, C16H21NO2 , and molecular mass of 259.343 g/mol is marketed as Rozerem by Takeda Pharmaceuticals North America. It is the first in a new class of sleep agents that selectively binds to the melatonin receptors in the suprachiasmatic nucleus (SCN), versus binding to GABA A receptors, such as with drugs like Ambien (zolpidem), eszopiclone, and zaleplon. Ramelteon is approved by the FDA for long-term use.
Ramelteon does not show any appreciable binding to GABAA receptors, which are associated with anxiolytic, myorelaxant, and amnesic effects.
Uses
Ramelteon is used for insomnia, particularly delayed sleep onset. Ramelteon has not been shown to produce dependence and has shown no potential for abuse, and the withdrawal and rebound insomnia that is typical with other GABA modulators is not present in ramelteon. It is currently the only non-scheduled prescription drug for the treatment of insomnia available in the United States.[1]
Mechanism of action
Ramelteon is a melatonin receptor agonist with both high affinity for melatonin MT1 and MT2 receptors and selectivity over the MT3 receptor. Ramelteon demonstrates full agonist activity in vitro in cells expressing human MT1 or MT2 receptors, and high selectivity for human MT 1 and MT2 receptors compared to the MT3 receptor.
The activity of ramelteon at the MT1 and MT2 receptors is believed to contribute to its sleep-promoting properties, as these receptors, acted upon by endogenous melatonin, are thought to be involved in the maintenance of the circadian rhythm underlying the normal sleep-wake cycle. Ramelteon has no appreciable affinity for the GABA receptor complex or for receptors that bind neuropeptides, cytokines, serotonin, dopamine, noradrenaline, acetylcholine, and opiates. Ramelteon also does not interfere with the activity of a number of selected enzymes in a standard panel.
The significance of ramelteon's lack of affinity for the MT3 receptor is not clear, despite the manufacturer's emphasis of this fact in commercial advertisements. The MT3 receptor appears almost exclusively in the gut and might not have any relationship to sleep or wakefulness.
The major metabolite of ramelteon, M-II, is active and has approximately one tenth and one fifth the binding affinity of the parent molecule for the human MT1 and MT2 receptors, respectively, and is 17 – 25-fold less potent than ramelteon in in vitro functional assays. Although the potency of M-II at MT1 and MT2 receptors is lower than the parent drug, M-II circulates at higher concentrations than the parent producing 20 – 100 fold greater mean systemic exposure when compared to ramelteon. M-II has weak affinity for the serotonin 5-HT2B receptor, but no appreciable affinity for other receptors or enzymes. Similar to ramelteon, M-II does not interfere with the activity of a number of endogenous enzymes. All other known metabolites of ramelteon are inactive.
No published studies have indicated whether ramelteon is more or less safe or effective than melatonin, a much less expensive drug, widely available in the United States without a prescription. The biological action of melatonin is similar to that of ramelteon. The purported advantage of ramelteon is that the product and dosage is more likely to be pure and standardized, because it is a prescription drug that is monitored by the Food and Drug Administration (FDA).
Drug interactions
Ramelteon has been studied in combination with omeprazole, theophylline, dextromethorphan, midazolam (although one would probably not come across this medicine due to its high clearance and shorter half-life than other benzodiazepines. Thus, Intensive Care Units must assess the patient and carefully administer as needed. It is also used as a sedative before operations. Its half-life is less or greater than one hour. It is usually used in an Intensive Care Unit and administered via IV due to the destructive nature of first pass metabolism.) Other such drug-drug interactions include digoxin and warfarin. There were no clinically meaningful effects when ramelteon was coadministered with any of these drugs.
A drug interaction study showed that there were no clinically meaningful effects or an increase in adverse events when ramelteon and the SSRI Prozac (fluoxetine) were coadministered. Ramelteon and Luvox (fluvoxamine) should not be coadministered.
Ramelteon should be administered with caution in patients taking other CYP1A2 inhibitors, strong CYP3A4 inhibitors such as ketoconazole, and strong CYP2C9 inhibitors such as fluconazole. Efficacy may be reduced when ramelteon is used in combination with potent CYP enzyme inducers such as rifampin, since ramelteon concentrations may be decreased.
Sources and external links
- Rozerem Official Website
- Prescribing Information Data Sheet
- RxList.com
- Clinical Pharmacokinetic Monitoring of Midazolam in Critically Ill Patients in relation to midazolam as a drug-drug interaction to Rozerem
References