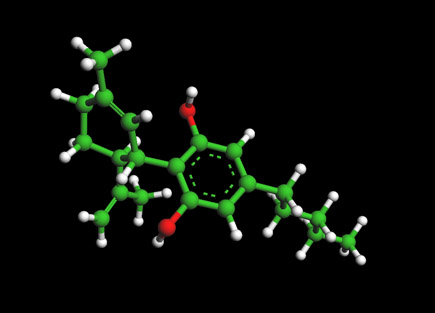
Taxol Molecule - Paclitaxel
Ball and Stick Model for Taxol Molecule - Paclitaxel
To View the Taxol Molecule in 3D --->>in 3D with Jsmol
Paclitaxel -- Taxol
Paclitaxel is a mitotic inhibitor used in cancer chemotherapy. It was discovered in a National Cancer Institute program at the Research Triangle Institute in 1967 when Monroe E. Wall and Mansukh C. Wani isolated it from the bark of the Pacific yew tree, Taxus brevifolia and named it 'taxol'. When it was developed commercially by Bristol-Myers Squibb (BMS) the generic name was changed to 'paclitaxel' and the BMS compound is sold under the trademark 'Taxol®'.
Paclitaxel is now used to treat patients with lung, ovarian, breast cancer, head and neck cancer, and advanced forms of Kaposi's sarcoma. Paclitaxel is also used for the prevention of restenosis. Paclitaxel works by interfering with normal microtubule growth during cell division. Together with docetaxel, it forms the drug category of the taxanes. It was the subject of a notable total synthesis by Robert A. Holton. As well as offering substantial improvement in patient care, paclitaxel has been a relatively controversial drug. There was originally concern because of the environmental impact of its original sourcing, no longer used, from the Pacific yew. The assignment of rights, and even the name itself, to BMS were the subject of public debate and Congressional hearings.
The plant screening program, isolation, and preclinical trials
In 1955 the National Cancer Institute (NCI) set up the Cancer Chemotherapy National Service Center (CCNSC) to act as a public screening centre for anti-cancer activity in compounds submitted by external institutions and companies[3] Although the majority of compounds screened were of synthetic origin, one chemist, Jonathan Hartwell, who was employed there from 1958 onwards, had had experience of natural product derived compounds and began a plant screening operation.[4] After some years of informal arrangements, in July 1960 the NCI commissioned USDA botanists to collect samples from about 1000 plant species per year.[5] On August 21st, 1962, one of those botanists, Arthur S. Barclay, collected bark from a single Pacific yew tree, Taxus brevifolia, in a forest north of the town of Packwood, Washington as part of a four month trip collecting material from over 200 different species.[6] The material was then processed by a number of specialist CCNSC subcontractors and one of the Taxus samples was found to be cytotoxic in a cellular assay on 22 May 1964.[7]
Accordingly, in late 1964 or early 1965, the fractionation and isolation laboratory run by Monroe E. Wall in Research Triangle Park, North Carolina, began work on fresh Taxus samples, isolating the active ingredient in September 1966 and announcing their findings at an April 1967 American Chemical Society meeting in Miami Beach.[8]. They named the pure compound 'taxol' in June 1967. [9] Wall and his colleague Wani published their results, including the chemical structure, in 1971.[10].
The NCI continued to commission work to collect more Taxus bark and to isolate increasing quantities of taxol. By 1969 28kg of crude extract had been isolated from almost 1,200kg of bark, although this ultimately yielded only 10g of pure material. [11] But for several years no use was made of the compound by the NCI. In 1975 it was shown to be active in another in vitro system ; two years later a new department head reviewed the data and finally recommended that taxol be moved on to the next stage in the discovery process. [12] This required increasing quantities of purified taxol, up to 600g, and in 1977 a further request for 7,000 pounds of bark was made. In 1978, two NCI researchers published a report showing that taxol was mildly effective in leukaemic mice. [13]
In November 1978, taxol was shown to be effective in xenograft studies.[14] Meanwhile taxol began to be well known in the cell biology, as well as the cancer community, with a publication in early 1979 by Susan B. Horwitz, a molecular pharmacologist at Albert Einstein College of Medicine, that showed that taxol had a previously unknown mechanism of action involving the stabilisation of microtubules. Together with formulation problems, this increased interest from researchers meant that by 1980 the NCI envisaged needing to collect 20,000 pounds of bark. [15]. Animal toxicology studies were complete by June 1982, and in November NCI applied for the INDA necessary to begin clinical trials in humans.[16].
Early clinical trials, supply and the transfer to BMS
Phase I clinical trials began in April 1984 and the decision to start Phase II trials was made a year later.[17] These larger trials needed more bark and collection of a further 12,000 pounds was commissioned, which enabled some phase II trials to begin by the end of 1986. But by then it was recognised that the demand for taxol might be substantial and that more than 60,000 pounds of bark might be needed as a minimum. This unprecedentedly large amount brought ecological concerns about the impact on yew populations into focus for the first time as local politicians and foresters expressed unease at the program[18].
The first public report from a phase II trial in May 1988 showed an effect in melanoma patients and a remarkable response rate of 30% in patients with refractory ovarian cancer.[19]. At this point Gordon Cragg of the NCI's Natural Product Branch calculated that the synthesis of enough taxol to treat all the ovarian cancer and melanoma cases in the US would require the destruction of 360,000 trees annually. For the first time, serious consideration was given to the problem of supply.[20]. Because of the practical and in particular the financial scale of the programme needed, the NCI decided to seek association with a pharmaceutical company, and in August 1989 it published a Cooperative Research and Development Agreement (CRADA) offering its current stock and supply from current bark stocks, together with proprietary access to the data so far collected, to a company willing to commit to providing the funds to collect further raw material, isolate taxol, and fund a large proportion of clinical trials. In the words of Goodman and Welsh, authors of a substantial scholarly book on taxol, [The NCI] was thinking, not of collaboration, ... but of a hand-over of taxol (and its problems) [21]
Although widely advertised, only four companies responded to the CRADA, including Bristol-Myers Squibb (BMS), who were selected as the partner in December 1989. The choice of BMS later became controversial and was the subject of Congressional hearings in 1991 and 1992. While it seems clear that the NCI had little choice but to seek a commercial partner, there was also controversy about the terms of the deal, eventually leading to a report by the General Accounting Office in 2003 which concluded that the NIH had failed to ensure value for money.[22] In related CRADAs with the USDA and Department of the Interior, Bristol-Myers Squibb were given exclusive first refusal on all Federal supplies of Taxus brevifolia. This exclusive contract lead to some criticism for giving BMS a "cancer monopoly."[23] Eighteen months after the CRADA, BMS filed a new drug application (NDA) which was given FDA approval at the very end of 1992. [24] Although there was no patent on the compound, the provisions of the Waxman-Hatch Act gave Bristol-Myers Squibb five years exclusive marketing rights.
In 1990, Bristol-Myers Squibb applied to trademark the name 'taxol' as Taxol®. This was controversially approved in 1992. At the same time, 'paclitaxel' replaced 'taxol' as the generic name of the compound. Critics, including the journal Nature, argued that the name taxol had been used for more than two decades and in more than 600 scientific articles and suggested that the trademark should not have been awarded and the BMS should renounce its rights to it.[25] BMS argued that changing the name would cause confusion among oncologists and possibly endanger the health of patients. BMS has continued to defend its rights to the name in the courts.[26] BMS have also been criticised for misrepresentation by Goodman and Walsh, who quote from a company report saying that It was not until 1971 that ... testing ... enabled the isolation of paclitaxel, initially described as 'compound 17'[27] This quote is strictly speaking accurate: the objection seems to be that this misleadingly neglects to explain that it was the scientist doing the isolation who named the compound taxol and it was not referred to in any other way for more than twenty years. Annual sales peaked in 2000, reaching US$1.6 billion; paclitaxel is now available in generic form.
Mechanism of action
Paclitaxel interferes with the normal function of microtubule growth. Whereas drugs like colchicine cause the depolymerization of microtubules, paclitaxel arrests their function by having the opposite effect; it hyper-stabilizes their structure. This destroys the cell's ability to use its cytoskeleton in a flexible manner. Specifically, paclitaxel binds to the ß subunit of tubulin. Tubulin is the "building block" of microtubules, and the binding of paclitaxel locks these building blocks in place. The resulting microtubule/paclitaxel complex does not have the ability to disassemble. This adversely affects cell function because the shortening and lengthening of microtubules (termed dynamic instability) is necessary for their function as a mechanism to transport other cellular components. For example, during mitosis, microtubules position the chromosomes during their replication and subsequent separation into the two daughter-cell nuclei.[34] Further research has indicated that paclitaxel induces programmed cell death (apoptosis) in cancer cells by binding to an apoptosis stopping protein called Bcl-2 (B-cell leukemia 2) and thus arresting its function. In addition to stabilizing microtubules paclitaxel may act as a molecular mop by sequestering free tubulin effectively depleting the cells supply of tubulin monomers and/or dimers. This activity may trigger the aforementioned apoptosis.[35] One common characteristic of most cancer cells is their rapid rate of cell division. In order to accommodate this, the cytoskeleton of a cell undergoes extensive restructuring. Paclitaxel is an effective treatment for aggressive cancers because it adversely affects the process of cell division by preventing this restructuring. Cancer cells are also destroyed by the aforementioned anti-Bcl-2 mechanism. Other cells are also affected adversely, but since cancer cells divide much faster than non-cancerous cells, they are far more susceptible to paclitaxel treatment.
Clinical use
Paclitaxel is approved in the UK for ovarian cancer, breast cancer, lung cancer. It is also used in the treatment of Kaposi's sarcoma.[36] It is recommended in NICE guidance of June 2001 that it should be used for non-small cell lung cancer in patients unsuitable for curative treatment, and in first-line and second-line treatment of ovarian cancer. In September 2001 NICE recommended that paclitaxel should be available for the treatment of advanced breast cancer after the failure of anthracyclic chemotherapy, but that its first-line use should be limited to clinical trials. In September 2006 NICE recommended that paclitaxel should not be used in the adjuvant treatment of early node-positive breast cancer.[37] The cost to the NHS per patient in early breast cancer, assuming four cycles of treatment, is about £4000.[38]
Similar compounds
The closely related taxane docetaxel has a similar set of clinical uses to paclitaxel. In January 2005, the Food and Drug Administration (FDA) approved Abraxane (protein-bound paclitaxel) for the treatment of breast cancer after failure of combination chemotherapy for metastatic disease or relapse within six months of adjuvant chemotherapy. In this preparation, paclitaxel is bonded to albumin as the delivery agent as an alternative to the often toxic, solvent delivery method.[39]
References
- Sandra Peltier, S.; Oger, J.-M., Lagarce, F.; Couet, W.; Benoît, J.-P. (June 2006). "Enhanced Oral Paclitaxel Bioavailability After Administration of Paclitaxel-Loaded Lipid Nanocapsules". Pharmaceutical Research 23 (6): 1243-1250. doi:10.1007/s11095-006-0022-2.
- (2001) "Refined structure of tubulin at 3.5 Ã… resolution". Journal of Molecular Biology 313 (5): 1045-m1057. doi:10.1006/jmbi.2001.5077.
- Goodman, Jordan; Walsh, Vivien (2001). The Story of Taxol: Nature and Politics in the Pursuit of an Anti-Cancer Drug. Cambridge University Press. ISBN 0 521 56123 X. , p17
- Goodman and Walsh, p22
- Goodman and Walsh p25, p28
- Goodman and Walsh, p51
- Goodman and Walsh, p51
- Wall ME, Wani MC (1995). "Camptothecin and taxol: discovery to clinic--thirteenth Bruce F. Cain Memorial Award Lecture". Cancer Res.55 (4): 753-60. PMID 7850785.
- Goodman and Walsh p51
- Wani M, Taylor H, Wall M, Coggon P, McPhail A (1971). "Plant antitumor agents. VI. The isolation and structure of taxol, a novel antileukemic and antitumor agent from Taxus brevifolia". J Am Chem Soc 93 (9): 2325-2327. PMID 5553076.
- Goodman and Walsh p81
- Goodman and Walsh p79, p81
- Fuchs, David A and Johnson, Randall K (1978). "Cytologic evidence that taxol, an antineoplastic agent from Taxus brevifolia, acts as a mitotic spindle poison". Cancer Treatment Reports 62: 1219-1222. PMID 688258.
- Goodman and Walsh 95
- Goodman and Walsh p97
- Goodman and Walsh p97
- Goodman and Walsh 115
- Goodman and Walsh 120
- Rowinsky, EK and others (1988). "Phase II study of taxol in advanced epithelial malignancies". Proceedings of the Association of Clinical Oncology 7: 136.
- Goodman and Walsh 120
- Goodman and Walsh p120
- Technology Transfer: NIH-Private Sector Partnership in the Development of Taxol.
- Nader, Ralph; Love, James. "Looting the medicine chest: how Bristol-Myers Squibb made off with the public's cancer research." The Progressive. February, 1993. Retrieved on March 9, 2007.
- Goodman and Walsh p120
- (1995) "Names for hi-jacking". Nature373 (6513): 370. doi:10.1038/373370a0. PMID 7830775.
- Goodman and Walsh p170
- Bristol-Myers Squibb, The development of Taxol®(paclitaxel), March 1997, as cited in Goodman and Walsh p2
- Goodman and Walsh pp172-175
- Goodman and Walsh pp100-101
- Stephenson, Frank (Fall). "A tale of taxol". Florida State University Research In Review 12.
- Phyton news release.
- 2004 Greener Synthetic Pathways Award: Bristol-Myers Squibb Company: Development of a Green Synthesis for Taxol® Manufacture via Plant Cell Fermentation and Extraction.
- Zhao, K.; et al. "Study on the Preparation and Regeneration of Protoplast from Taxol-producing Fungus Nodulisporium sylviforme'." Nature and Science. 2004. 2 (2). pp. 52-59.
- Kumar, N. "Taxol-induced Polymerization of Purified Tubulin." Journal of Biological Chemistry. 1981. Vol. 256, No. 20, 10435-10441.
- Foss M, Wilcox BWL, Alsop GB, Zhang D (2008) Taxol Crystals Can Masquerade as Stabilized Microtubules. PLoS ONE 3(1): e1476 doi:10.1371/journal.pone.0001476
- Saville M, Lietzau J, Pluda J, Feuerstein I, Odom J, Wilson W, Humphrey R, Feigal E, Steinberg S, Broder S (July 1 1995). "Treatment of HIV-associated Kaposi's sarcoma with paclitaxel.". Lancet 346 (8966): 26-8. PMID 7603142.
- British National Formulary.
- NICE Guidance TA108.
- "Abraxane Drug Information." Food and Drug Administration. January 7, 2005. Retrieved on March 9, 2007.
- Heldman A, Cheng L, Jenkins G, Heller P, Kim D, Ware M, Nater C, Hruban R, Rezai B, Abella B, Bunge K, Kinsella J, Sollott S, Lakatta E, Brinker J, Hunter W, Froehlich J (2001). "Paclitaxel stent coating inhibits neointimal hyperplasia at 4 weeks in a porcine model of coronary restenosis.". Circulation 103 (18): 2289-95. PMID 11342479.
- "Medline Plus Entry for Taxol." MEDLINE. Last revised on April 1, 2003. Retrieved on March 9, 2007.
External links
- NCI Drug Information Summary for Patients.
- NCI Drug Dictionary Definition
- Molecule of the Month: TAXOL by Neil Edwards, University of Bristol.
- A Tale of Taxol from Florida State University.
- Anzatax / Paclitaxel Virtual Cancer Centre
Molecules of Life Resources
The Cannabidiol Molecule
Cannabidiol (CBD is the major non-psychoactive component of Cannabis and is being looked at by major drug and consumer companies for various medical and social uses.